What causes Gallstones?
The Gallbladder is a sac, which stores bile and lies beneath the liver. Bile is made by the liver and contains bile pigments, bile salts, lipids and cholesterol and is released into the duodenum (first part of the small bowel) to help digest fats. Gallstones can form in the Gallbladder due to an imbalance in the constituents of bile, therefore predominantly are made of bile pigments and/or cholesterol but are commonly mixed stones. The large majority of patients with gallstones have little or no symptoms. If symptoms do present from gallstones they are usually as a result of complications of gallstones and are described below.
Who commonly presents with Gallstones?
Gallstones are associated with women more than men (Fair, Fertile, Female's in their Forties). Gallstones occur in approximately 20% of women and 12% of men (this may be because the female hormones cause more cholesterol to be excreted in the bile).
However, the majority of patients with gallstones do not require any treatment with only 20% of patients undergoing surgery.
Any individual can develop Gallstones but factors, which increase the risks, include:
* Patients with diabetes
* Undergoing obesity surgery
* Use of the oral contraceptive pill
* Pregnancy
* Overweight and obese individuals
* Certain blood disorders (Haemolytic Anaemia)
* Inflammatory bowel disease (Crohn's).
* Age - chance of developing gallstones increases with age
* Ethnicity - American Indians have the highest incidence of gallstones in the world
How do Gallstones present?
Gallstones as mentioned may not cause any symptoms and only discovered by chance while testing for other conditions. They can however, cause symptoms such as:
Biliary Colic - 'Sharp intense abdominal pain' - this is pain experienced predominantly in the upper right abdomen. The pain is usually constant in nature, can also radiate through or around to the back and in between the shoulder blades which can last from between 1 to 3 hours. The pain can also be associated with nausea. The symptoms of biliary colic are commonly associated with and brought on by the consumption of 'fatty' or rich foods.
Sometimes gallstones may present with symptoms of chronic indigestion, which may include abdominal bloating, flatulence and nausea especially after a fatty meal. However these symptoms may also be associated with gastro-oesophageal reflux.
Acute cholecystitis - 'Fever, sickness and abdominal pain' - Gallstones can also cause acute inflammation/ infection of the Gallbladder. Acute cholecystitis will present with symptoms of pain as well as a fever and sweating.
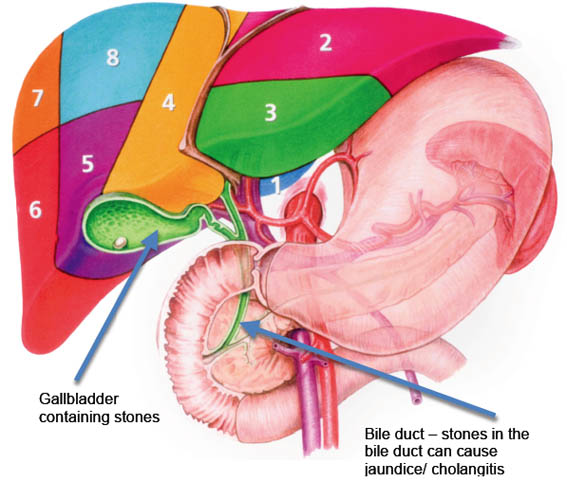
Jaundice - 'Yellow discolouration of the skin' - this is yellow skin discolouration, which occurs when a stone from the gallbladder enters the main bile duct and is unable to pass through into the duodenum (see diagram). Jaundice can present with a fever and generally feeling unwell and is described as cholangitis. A simple specialised camera test called an ERCP (Endoscopic Retrograde Cholangio-pancreatography) is required to remove the stone but most patients can safely undergo removal of the stone by keyhole surgery at the same time as the gallbladder is removed, laparoscopic cholecystectomy with bile duct exploration (see bile duct stones).
Acute pancreatitis - 'Intense abdominal pain with vomiting' - small gallstones or 'sludge' can pass into the bile duct and block the main pancreas duct resulting in acute pancreatitis. This is a condition that usually presents with severe abdominal pain, nausea and vomiting. Pancreatitis tends to be treated in hospital with painkillers and fluids to allow the symptoms to settle, following which, at an appropriate time the gallbladder is removed, by keyhole surgery.
What can I eat if I have Gallstones?
'Fatty' or 'rich foods' (high in cholesterol) can bring on the symptoms of Gallstones as described above. Do not over eat these and try and eat fresh food and fruit as much as possible.
Do's | Dont's |
Salad
Fresh Fruit
Fish
Tomatoes
Fresh Vegetables
| Egg's
Chocolate
Spicy Food
Cheese
Other Dairy products
Cakes and Biscuits |
How are Gallstones diagnosed?
Your surgeon will be able to diagnose if you have gallstones based on the symptoms described above. If gallstones are suspected then further tests as outlined below will be required (also see Diagnostics)
Ultrasound: The most sensitive test performed when gallstones are suspected is the ultrasound examination. An ultrasound machine uses sound waves to create images of the gallbladder and other organs in the abdomen. The sound waves from the machine bounce off gallstones if present and the images are captured on a video monitor.
Magnetic resonance cholangiogram (MR scan): is used to diagnose suspected bile duct stones. It is non-invasive and is used when the suspicion of bile duct stone is high.
Endoscopic Ultrasound (EUS): can be used to diagnose stones from the bile duct as well as biliary sludge. It involves passing a flexible camera tube down the oesophagus (food pipe) and into the small intestine (duodenum). The flexible camera has an ultrasound probe at its tip, which can accurately diagnose stones both in the gallbladder and the bile ducts. It is sometimes combined with an ERCP, which is designed to remove bile duct stones.
Computed tomogram (CT/ CAT scan): sometimes is used mainly in the evaluation of complications of gallstones such as pancreatitis.
How are Gallstones treated?
Laparoscopic Cholecystectomy (with on table cholangiogram)
Once Gallstones are diagnosed keyhole surgery, Laparoscopic Cholecystectomy, is recommended to remove the gallbladder. Surgery is performed under a general anaesthetic using three, four or sometimes a single incision on the abdominal wall (SILS - single incision laparoscopic surgery) (click here for diagrams). A miniature camera and specially designed instruments are used. The abdominal organs are inspected and the gallbladder identified. A special X-ray of the bile ducts is routinely performed in all patients if possible (cholangiogram) to ensure the anatomy is clearly identified, there are no stones in the bile duct which may require further treatment and above all it has been shown to reduce the risk of potential complications (Flum et al JAMA 2003). All surgery is performed inside the abdomen with the entire gallbladder containing the stones removed. The skin is closed using dissolving stitches. In some people there may be some minor bruises in the first week, which usually settles down.
The advantages of laparoscopic approach include:
* Less postoperative pain
* Reduced hospital stay
* Quicker physical recovery
* Less wound scarring
Occasionally as happens in 2% of patients, it may not be possible to complete the procedure using the keyhole approach. The operation will therefore be converted to an open procedure. Your surgeon will discuss this with you prior to surgery.
Laparoscopic cholecystectomy is the treatment of choice for all patients presenting with any of the complications of gallstones described above from biliary colic to acute cholecystitis.
What are the main risks of surgery?
Your surgeon will advise on any specific complications and risks. For all types of surgery there is always a risk of wound infection. Specifically for laparoscopic cholecystectomy there is always a small risk of undergoing an open operation instead of keyhole in 2% of patients and a risk of bile duct injury of <0.3% (National quoted figure). Your surgeon will discuss this with you prior to surgery.
What happens after surgery?
You will be able to eat and drink after your operation. The operation is usually straightforward and most people are usually well enough to go home within twenty-four hours. Most people should be well enough to engage in gentle sporting activities in 7 to 10 days.
There is no special dietary restriction following gallbladder removal and you can live without your gallbladder. In a small minority of individuals (1%), there may be increased bowel frequency following gallbladder removal because bile flows directly into the intestine from the liver but this usually settles down most of the time.
Driving can be resumed after 7days but do check with your insurance company first for appropriate cover.
Most patients fully recover from surgery within two to three weeks.
SILS - Single Incision Laparoscopic Surgery
This is a relatively new procedure, which utilises the insertion of a special instrument into the umbilicus 'belly button' and allows the surgeons to carry out the entire operation through this 'single hole'. This technique at present can be offered to patients and the surgeon will discuss with you if your are suitable. At present there is no overwhelming clinical data to suggest its routine use or benefits over the traditional approach and Manchester general surgery's experience has demonstrated that patients largely benefit from the cosmetic result of a single wound/ scar. Please advise your surgeon if you would like more information on this procedure.
Incisions used for laparoscopic cholecystectomy
Diagram of abdomen shown below
A: Traditionally four incisions are used for this procedure
B: In some patients only three small 5mm incisions can be used
C: In selective cases the procedure can be performed through a single incision (SILS - single incision laparoscopic surgery)
For your patient information please click here
References:
Flum et al. JAMA 2003; 289(13): 1639-1644
Gallbladder Surgery Diagram